Therapy with tPA Found to Be Safe in SCD Patients Who Have a Stroke
Patients who suffered a stroke and have sickle cell disease (SCD) can safely receive lytic therapy with tissue plasminogen activator (tPA), according to new research.
The study, “Coexistent Sickle Cell Disease Has No Impact on the Safety or Outcome of Lytic Therapy in Acute Ischemic Stroke,” was published in the journal Stroke.
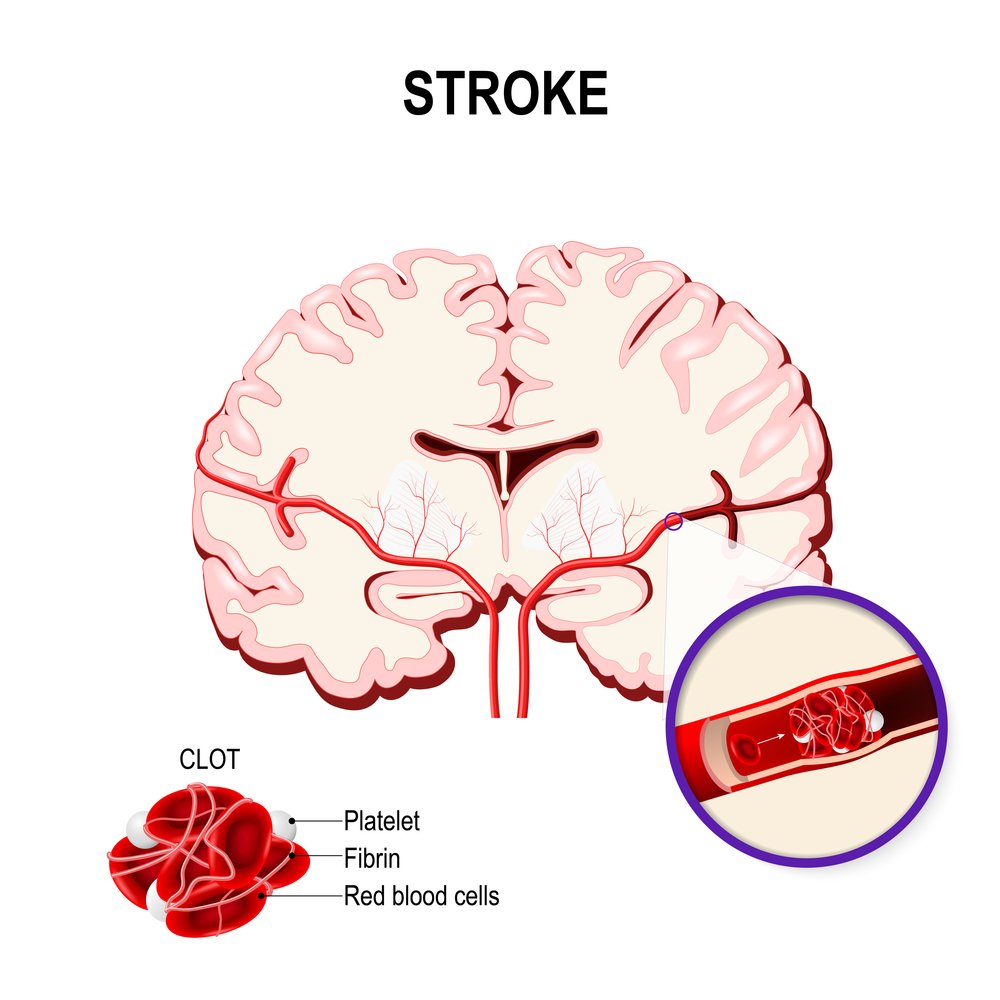
tPA is used to treat adults with ischemic stroke, a serious condition caused when a blood vessel carrying blood to the brain is blocked. tPA increases the ability of the body to dissolve clots, improving blood flow to the brain.
Stroke is an important complication of SCD, but the underlying mechanism of stroke in these patients is different: Here, the cause is not a blood clot, but instead the enhanced adhesion of the red blood cells to the blood vessel wall (endothelium).
SCD is not considered a contraindication to the use of tPA; however, the National Heart Lung and Blood Institute of the National Institutes of Health recommended red cell transfusions for stroke in sickle cell patients instead of tPA. Overall, the use of tPA in SCD was poorly established.
A team of researchers at the Medical University of South Carolina and colleagues at other institutions analyzed in-hospital data of stroke patients compiled in the Get With The Guidelines — Stroke database. In total, they reviewed 2,016,652 stroke patients who were patients at 1,952 U.S. hospitals between 2008 and 2015.
A total of 832 patients were found to have SCD and when the researchers compared the use of tPA between these patients and matched controls without SCD for age, gender, and race, they found no statistically significant differences: 8.2% for SCD patients vs. 9.4% for non-SCD patients. The same pattern of no significant differences was detected for timeliness of tPA administration (door-to-needle time, 73 minutes for SCD patients compared to 79 minutes for non-SCD patients), and rate of in-hospital complications.
An important parameter evaluated was the risk of intracranial hemorrhage, a rare but potentially fatal complication of tPA. From the total pool of patients treated with tPA, 4.9% of those with SCD suffered intracranial hemorrhage, while only 3.2% of those without SCD experienced this severe complication. The difference was not statistically significant, but still the increase in SCD patients is a warning sign for careful vigilance.
Other parameters analyzed included the overall rate of complications, in-hospital mortality and length of stay over four days, which showed no statistical differences between both groups.
“Having sickle cell disease did not adversely affect any of the indicators we measured,” Robert J. Adams, MD, distinguished professor of neurology and director of the South Carolina Center for Economic Excellence in Stroke, and the study’s first author, said in a press release.
“People with sickle cell disease and an acute stroke who would otherwise qualify for tPA did not have worse outcomes than stroke patients who did not have sickle cell disease,” he said.
Overall, these findings suggest that tPA is safe in patients with SCD and it may represent an additional therapeutic strategy to implement with the standard, red blood cell exchange for ischemic stroke in patients with SCD. Researchers wrote, however, that additional studies are needed to investigate other SCD-related care practices.
“These findings suggest that a future randomized trial that compares using red-blood cell exchange alone vs. combination therapy with tPA and red-blood cell exchange should be undertaken to evaluate the outcomes of [ischemic stroke] in patients with sickle cell disease,” said Julie Kanter, MD, director of Sickle Cell Research and a specialized SCD specialized hematologist.