Delta-aminolevulinate Molecule May Be Potential New Therapy for Sickle Cell Anemia, Study Suggests
Treatment with delta-aminolevulinate (ALA), a precursor of heme — the part of hemoglobin that carries oxygen — could be a future therapy option for people with sickle cell anemia and β-thalassemia, a recent study suggests.
The study, “δ-Aminolevulinate induces fetal hemoglobin expression by enhancing cellular heme biosynthesis,” was published in the journal Experimental Biology and Medicine.
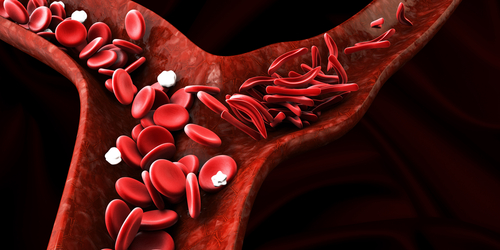
Adult hemoglobin consists of four protein subunits: two alpha-globin and two beta-globin. A ring-shaped molecule called heme attaches to each of these protein subunits and an iron atom at its center binds the oxygen people breath. The iron and oxygen in heme give blood its bright red color.
Mutations in the HBB gene, which makes beta-globin, cause sickle cell disease and β-thalassemia.
A different type of hemoglobin, called fetal hemoglobin (HbF), is present only in the fetus and newborn. It is composed of two alpha and two gamma subunits. Compared with the adult form of hemoglobin, HbF is more effective in binding and carrying oxygen around the body.
Increasing the levels of fetal hemoglobin can improve the clinical symptoms of sickle cell disease. Hydroxyurea, the first FDA-approved medicine for SCD, works by increasing HbF levels. However, a significant number of individuals do not respond to therapy with hydroxyurea, so new medicines are urgently needed.
The first step in the synthesis of the heme group is the production of a compound called delta-aminolevulinate (ALA), a type of amino acid, which are the building blocks of proteins. This is the rate-limiting step, meaning that it is the slowest, and the overall rate of all other reactions in the pathway depend on it.
Scientists in the department of biological sciences at the University of Texas at Dallas tried adding ALA to a human erythroid cell line — the lineage of cells that eventually gives rise to red blood cells — to bypass the initial rate-limiting step. They found that the expression of the gamma-globin gene increased two-fold and HbF production more than tripled. Meanwhile, beta-globin expression did not significantly change.
Similar effects were seen with erythroid progenitors generated from human stem cells, which more closely resemble the progenitors which give rise to red blood cells.
This is important because only HbF production was enhanced, not synthesis of the adult beta-globin subunit, suggesting that it could have a beneficial effect in SCD.
Mechanistic studies determined that enhanced heme biosynthesis and reactive oxygen species partly explained the increased production of HbF.
“These data support future study to explore the potential of stimulating intracellular [inside the cells] heme biosynthesis [production] by ALA or similar compounds as a novel therapeutic strategy for treating SCD and β-thalassemia,” the study concluded.
“These results support future studies to explore the potential of stimulating intracellular heme biosynthesis by ALA or similar compounds as a novel therapeutic strategy for treating SCD and beta-thalassemia,” Li Liu, PhD, the lead investigator, said in a press release.
“Researchers in the sickle cell field are currently pursuing many clinical trials that would expand the FDA approved SCD therapeutic choices beyond Hydroxyurea, and the more recently approved Endari. Liu et al have provided in vitro [in the lab] evidence that ALA, through induction of heme biosynthesis, should be considered as a possible future therapeutic option,” said Steven R. Goodman, PhD, editor-in-chief of Experimental Biology & Medicine.