Pediatric SCD Patients with Acute Kidney Injury Face More Hospital Care, Higher Costs, Large–scale Analysis Finds
Written by |
Pediatric patients with sickle cell disease complicated by acute kidney injury (AKI) were more likely to be admitted to the intensive care unit (ICU), had longer hospital stays, accumulated greater hospitalization costs, and had a higher rate of readmission, a large-scale analysis found.
Increasing age at hospital admission and a history of high blood pressure and blood in the urine were identified as risk factors for AKI.
The study also found that those receiving hydroxyurea — a cancer medicine — were more protected from this complication.
The study, “Acute kidney injury in paediatric patients with sickle cell disease is associated with increased morbidity and resource utilization,” was published in the British Journal of Haematology.
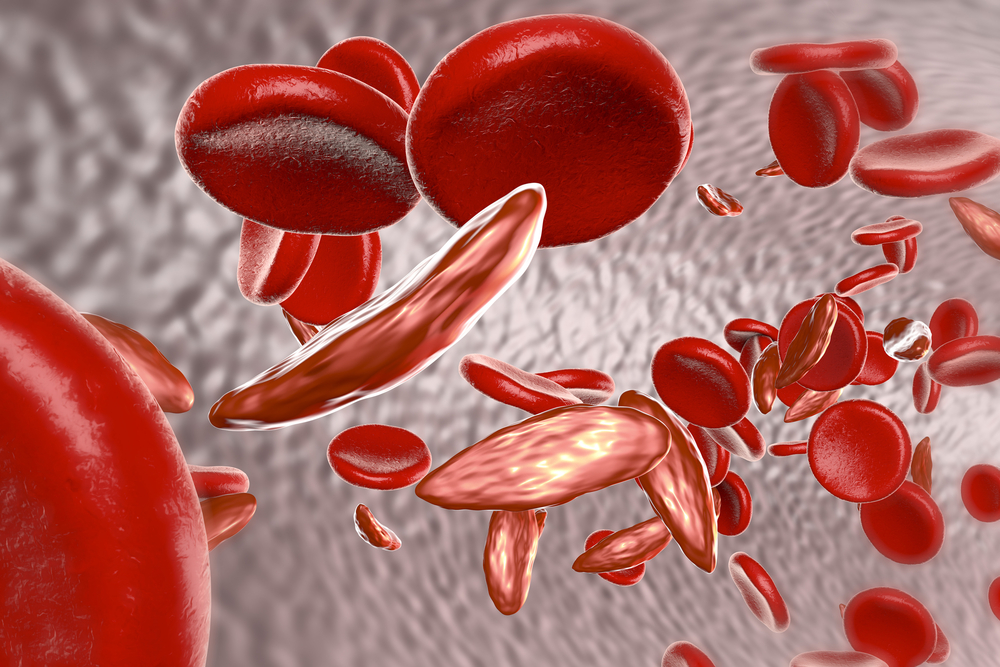
Kidney disease is a common complication in people with sickle cell disease, known as SCD. A sudden episode of kidney failure or kidney damage — known as acute kidney injury — can impact both short-term and long-term SCD patient outcomes.
In adults with the disease, being admitted to the hospital with AKI complications has been linked to longer hospital stays, unfavorable outcomes for those requiring intensive care, high admission costs, and an increased risk of mortality.
However, studies reporting on the outcomes of pediatric SCD patients who were admitted to hospital with AKI are limited.
To get a clearer picture, a team of investigators based at the University of Pittsburgh Medical Center (UPMC) Children’s Hospital of Pittsburgh analyzed the medical records of those with SCD under the age of 22 who were admitted and discharged from the hospital following a vaso-occlusive pain crisis (VOC). Such crises are common complications for SCD patients, caused by the obstruction of sickled red blood cells.
Demographic information from the first VOC was collected, including age, gender, ethnic origin, insurance payer, SCD type, and income.
The analysis focused on variables such as the need for ICU care, readmission within seven days, hospitalization costs, length of stay, and medication use.
Other SCD-related conditions included in the analysis were high blood pressure, pulmonary hypertension, stroke, chronic kidney disease, high levels of urine protein or proteinuria, blood in the urine or haematuria, pneumonia, and acute chest syndrome, marked by pain, cough, and fever.
The patients were divided into two groups, one comprised of those with AKI complications and the other without.
The team identified 13,753 SCD patients from a total of 72,202 discharges, in which 188 (around 1.4%) had at least one admission complicated by AKI. The individuals who experienced AKI tended to be adolescents or young adults, as opposed to children.
Most of those with AKI complications carried the double HgbSS genotype — a defective gene inherited from both parents — and had twice as many hospital discharges during the study period compared with those without AKI.
Among the total hospital discharges, 2.5% were complicated by AKI, the analysis showed. Patients who experienced AKI were more likely to be admitted to the ICU, had a longer hospital stay (four days versus three days), accumulated higher hospitalization costs, and had a higher rate of readmission within seven days.
With the exception of pulmonary hypertension, all of the SCD-related co-conditions occurred more frequently in those with the AKI complication. In particular, acute chest syndrome was present in 53% of AKI cases.
A risk factor analysis found that increasing age and a history of high blood pressure and blood in the urine increased the risk of AKI. Patients with chronic kidney disease were over 20 times more likely to develop AKI compared with those without that secondary illness.
A history of taking the SCD medicine hydroxyurea (hydroxycarbamide) was protective against AKI, the researchers found. Those receiving this therapy were 36% less likely to develop acute kidney injury.
“The results of this study generate valuable information regarding the risk of AKI, risk factors for AKI development and the impact of AKI on care in paediatric patients with SCD,” the investigators said. “Episodes of AKI during hospitalization in children with SCD are associated with increased morbidity and utilization of hospital resources.”
“Increasing the use of hydroxycarbamide may decrease the likelihood of this complication,” they recommended.


