Abnormal Red Blood Cells’ Shape Affect Blood Clot Formation, Study Shows
Written by |
Abnormal sickle-shaped red blood cells characteristic of sickle cell disease (SCD) change the structure and dynamics of blood clots’ formations in veins, a study in mice and human blood shows.
Such changes may explain why SCD patients are at higher risk for venous thromboembolisms.
The study with those findings, “Red blood cells modulate structure and dynamics of venous clot formation in sickle cell disease,” was published in Blood.
SCD is a rare genetic disorder caused by mutations in the HBB gene, which provides instructions to make hemoglobin, a protein responsible for blood oxygen transport.
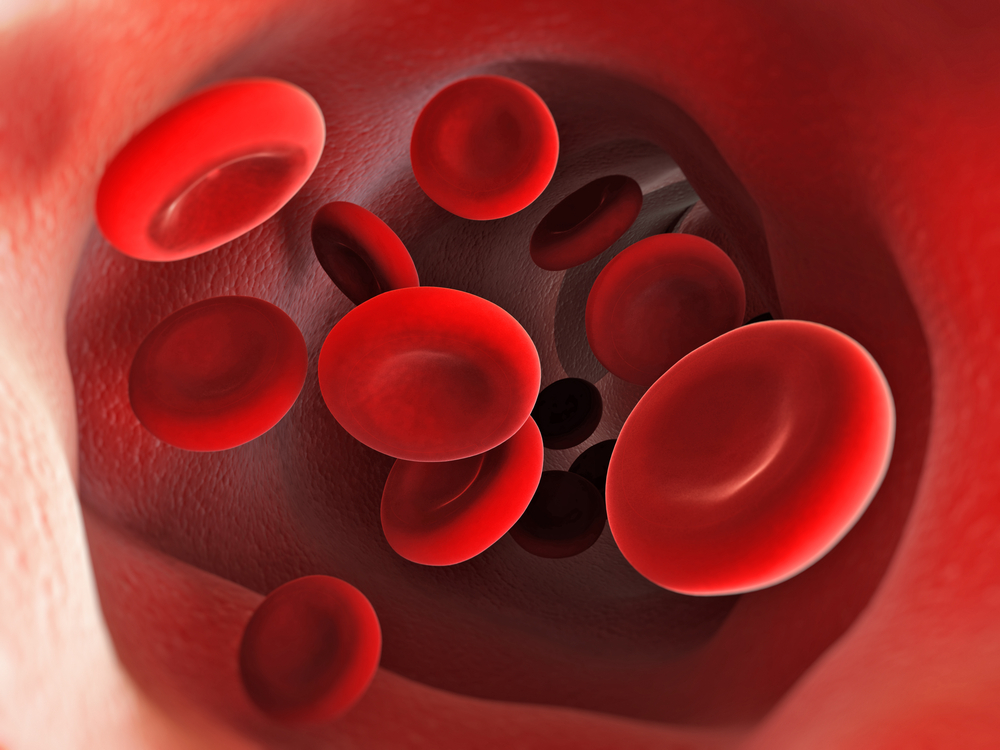
The red blood cells of SCD patients have an unusual sickle-like appearance caused by the production of abnormal hemoglobin, and tend to stick to one another, forming blood clots that hinder blood circulation.
For this reason, SCD patients have increased risks of developing venous thromboembolism (VTE, a blood clot that forms in a vein and can cause a heart attack or stroke) and other complications arising from excessive blood clotting.
Because sickle-shaped red blood cells are stiffer than normal disc-shaped red blood cells, “it would be expected that SCD might affect the properties of the clot.”
In this study, researchers set out to investigate how the different features of abnormal sickle-shaped red blood cells might affect the structure, properties and formation of blood clots in a mouse model of SCD and in blood samples from SCD patients.
First, they observed that vein blood clots from the animals with SCD were extremely dense and contained higher levels of fibrin (a protein involved in blood clotting) compared to blood clots in healthy animals.
Then the researchers decided to assess how red blood cells’ shape might affect blood clot contraction. In normal conditions, clot contraction is a process in which blood clots are “squeezed” and become smaller and more compact, to promote wound healing and normalize blood circulation. It is mediated by platelets (small cells responsible for blood clotting) and fibrin.
When researchers mimicked blood clot contraction ex vivo (an experiment performed outside the body of the animal), they found that, compared to SCD mice, a much higher number of red blood cells managed to escape from blood clots of healthy animals when they were “squeezed” The same happened in blood samples taken from SCD patients.
In normal conditions, the number of red blood cells that remain inside blood clots during contraction depends on how “tight” fibrin molecules are bound to each other. This is mediated by an enzyme, called factor XIIIa or fibrin stabilizing factor.
Interestingly, when investigators used an inhibitor of factor XIIIa in blood samples from healthy mice, they found that even more red blood cells managed to escape from blood clots during contraction. In SCD animals, however, red blood cells remained trapped inside the blood clot.
Anti-sickling compounds, including hydroxyurea that is normally used to treat pain crises associated with excessive blood clotting in SCD patients, failed to reduce red blood cells’ entrapment inside blood clots from SCD animals and patients.
Conversely, when they used an inhibitor of phosphatidylserine — a component of cell membranes that is found on the surface of red blood cells of SCD patients — they managed to increase the number of red blood cells that were able to escape from blood clots of SCD animals and patients.
Further analysis also revealed that blood clots from SCD patients formed from whole blood, but not plasma (liquid portion of the blood), were more resistant to fibrinolysis (the process by which fibrin molecules start to detach from each other inside blood clots). That suggested the cellular fraction in the patients’ blood was enhancing clots’ resistance to fibrinolysis.
Remarkably, red blood cells’ exchange (a therapeutic procedure in which patients’ red blood cells are replaced) normalized both fibrinolysis and blood clot contraction in SCD patients.
“Our data demonstrate that sickle RBCs [red blood cells] alter the structure and dynamics of venous clot formation. It is currently unknown whether long-term RBC exchange, which normalizes clot contraction and reverses resistance of sickle clots to fibrinolysis, mitigates the risk of VTE in SCD. Future clinical studies are needed to examine these possibilities,” the scientists concluded.