Hematology Society Releases Guidelines for Blood Transfusions in SCD
The American Society of Hematology released new clinical guidelines on the use of blood transfusions in people with sickle cell disease (SCD).
The transfusion guidelines are the second in a series of five therapy guidelines ASH is developing for SCD. Guidelines for managing heart and kidney disease in SCD were released last year.
The guidelines were described in the study, “American Society of Hematology 2020 guidelines for sickle cell disease: transfusion support,” published in the peer-reviewed journal Blood Advances.
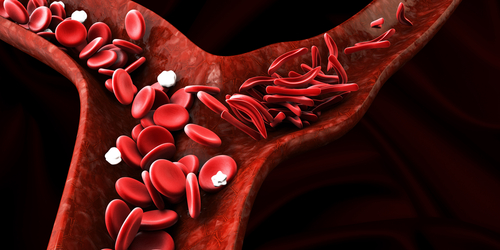
Blood transfusions are commonly used to manage SCD. But these procedures are not without risk. In fact, blood transfusions can lead to a series of complications, including immunological reactions and iron overload (excessive accumulation of iron in the body).
The guidelines, developed by an interdisciplinary team of clinicians, researchers, and patient representatives, aim to provide direction on the specific indications, mode of administration, prevention, and management of complications associated with blood transfusions.
“The ASH guidelines took the latest evidence into account to make recommendations that will help physicians and caregivers standardize and advance their patients’ care and decrease side effects,” Stella T. Chou, MD, a professor at Children’s Hospital of Philadelphia and co-chair of the team, said in a press release.
“We’ve also provided best practices and tips for patients and caregivers to help inform conversations with their healthcare providers,” Chou said. “ASH believes it is essential to provide updated treatment guidelines that reflect this increased knowledge and can help the medical community better treat SCD.”
One of the guidelines suggests that clinicians perform extended blood type matching to avoid immunological responses following blood transfusions.
Blood cells express certain proteins, called antigens, which are detected by the immune system. ABO antigens, which are associated with a particular blood type (A, B, AB, or O) and the RhD antigens, for which an individual can be deemed “positive” or “negative” are the most well-known.
There are many other types of blood antigens that are less familiar, in large part because they are less likely to trigger immune responses. However, in patients with SCD, it may be necessary to match these additional blood antigens in order to minimize the likelihood of an immunological reaction, ASH said.
The guidelines also recommend the use of treatments that suppress the immune system in people who have, or are at risk of having, those responses.
The guidelines also suggest that red cell exchange — a procedure in which only the oxygen-carrying red blood cells of a patient are replaced with those from a donor — is preferable to a simple blood transfusion, particularly in individuals with acute chest syndrome or those receiving chronic transfusions.
Transfusions should be given before surgery to those with SCD who will remain under general anesthesia for more than one hour, according to the recommendations. ASH also suggests that pregnant women receive blood transfusions in accordance with standard-of care-guidelines.
The guidelines also recommend additional screenings to assess iron levels in SCD patients requiring chronic transfusions.
The panel said most of its recommendations are “conditional,” as in many cases, there isn’t much available evidence regarding “outcomes of interest.”
“The limitations of these guidelines are inherent in the low or very low certainty of the evidence identified for many of the questions,” the committee said.
The authors also noted that several of their recommendations have “moderate resource implications.” In other words, costs — both financial and otherwise — may prove to be a barrier for some people receiving care based on these recommendations.






