Stem Cell Transplant, Gene Therapy in SCD Tied to Improved Quality of Life
Written by |
The quality of life of people with sickle cell disease (SCD) and transfusion-dependent thalassemia (TDT) — two inherited blood disorders — tends to improve if they receive a stem cell transplant or gene therapy, a review study found.
The study, “A systematic review of quality of life in sickle cell disease and thalassemia after stem cell transplant or gene therapy,” was published in the journal Blood Advances.
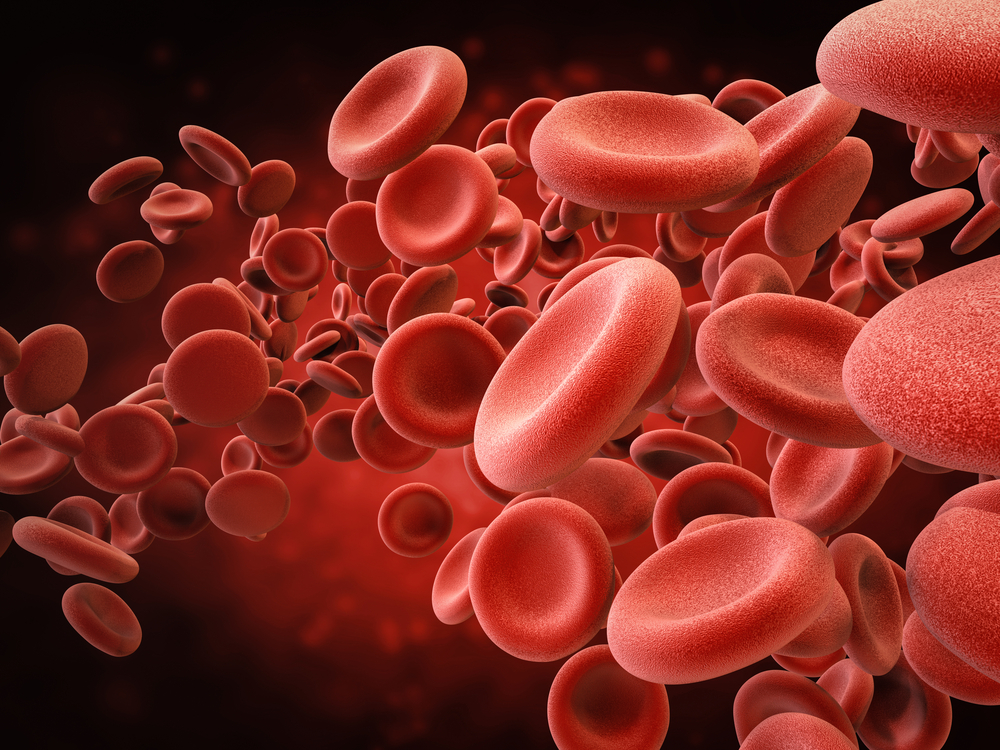
SCD and thalassemia are both blood diseases resulting from genetic mutations that cause defects in hemoglobin, the protein carrying oxygen in red blood cells. Both disorders can cause multiple complications for patients, and are known to have a negative impact on several aspects of quality of life, including mental, physical, and psychosocial well-being.
In recent years, there has been increasing interest in gene therapies and stem cell transplants, due to their curative potential. With gene therapy, there is the possibility of curing both disorders, stemming from the treatment’s ability to correct the mutations leading to hemoglobin defects. Meanwhile, a stem cell transplant has the ability to replace faulty blood cell progenitors, which give rise to unhealthy red blood cells, with healthy ones.
Despite their curative potential, the effects of these therapies on different aspects of an SCD or TDT patient’s quality of life are still poorly understood.
Now, researchers conducted a systematic literature review that aimed to gather and summarize the findings of studies investigating the impact of gene therapy and stem cell transplant on the health-related quality of life, or HRQOL, of patients with these two disorders.
After completing a thorough literature search using two large online databases — PubMed and the Cochrane Central Register of Controlled Trials — the investigators identified a total of 230 potentially relevant studies.
After removing duplicates and ones that did not meet certain inclusion criteria, the researchers selected a total of 16 studies to be included in the analyses. Nine involved patients with TDT, six focused on those with SCD, and one included both diseases. Altogether, these studies had enrolled a total of 517 participants — 416 with TDT and 101 with SCD.
Analyses showed that stem cell transplants were linked to small- to large-scale positive effects in most HRQOL domains, including physical and social areas.
In TDT patients, a stem cell transplant was often associated with large positive effects on both physical and emotional domains of HRQOL. Among people with SCD, the procedure was associated with large positive effects on all HRQOL domains.
Now the remaining question is how long those positive effects continue after the treatment.
“[Stem cell transplant] has a positive impact on several HRQOL domains in patients with SCD and thalassemia; however, more longitudinal studies are warranted to assess the sustainability of these effects,” the researchers wrote.
The potential benefits of gene therapy on patients’ HRQOL were more limited, yet still promising in both disorders. Two studies in people with TDT indicated that their overall quality of life improved after receiving gene therapy and they no longer required blood transfusions. Another two studies, these involving SCD patients, also found that gene therapy was associated with positive effects on several HRQOL domains, including pain intensity, physical function, depression, anxiety, and fatigue.
“Emerging data suggest improvement in HRQOL outcomes across different domains following gene therapy in thalassemia and SCD,” the investigators wrote.
They also added that future studies investigating the possible benefits of both therapies for patients’ quality of life are important and should rely on solid and validated measures to reach their conclusions.
“By understanding HRQOL outcomes after [stem cell transplant] and gene therapy, patients can be offered more insight to help them in the decision-making process regarding interventions,” the researchers wrote.
“Therefore, assessing HRQOL outcomes using reliable and valid generic and/or disease-specific measures in all future prospective [stem cell transplant], gene therapy or gene-editing trials is essentially needed,” they concluded.