Stem Cells from Half-Matched Donors in New Approach Reported to Cure 7 Sickle Cell Patients
Written by |
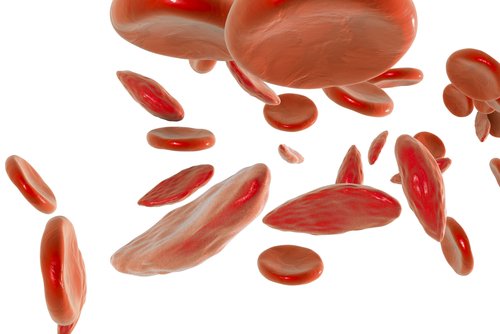
Under a new treatment protocol, seven adults with sickle cell anemia were treated — and reportedly cured — using stem cells from donors previously seen as incompatible.
The study reporting these treatments, “Haploidentical Peripheral Blood Stem Cell Transplantation Demonstrates Stable Engraftment in Adults with Sickle Cell Disease,” was published in the journal Biology of Blood and Marrow Transplantation. Its Chicago researchers recommend the protocol be tested in large-scale clinical trials.
Two people who share the same human leukocyte antigens (HLA) are said to “match,” which means that their tissues are compatible. These antigens are proteins located on the surface of most cells in the body, and are used by the immune system to recognize which cells belong to a person and which do not.
As HLA markers are inherited, close relatives are most likely to be good matches. This is key for transplants, as matching HLA markers between patient and donor reduce the risk of donor-cell rejection. However, only 20% of sickle cell patients have a fully-matched family member.
Previously, only fully-matched donors could be stem cells donors for patients with aggressive sickle cell anemia. Doctors at University of Illinois Hospital developed a protocol requiring only half-matching HLA markers and using a limited dose of chemotherapy.
“We have made great strides curing adults with sickle cell disease with stem cell transplants, but the unfortunate truth is that the majority of these patients have, until now, been unable to benefit from this treatment because there are no fully-matched HLA-compatible donors available in their family,” Damiano Rondelli, MD, the study’s senior author, said in a press release.
Between January 2014 and March 2017, a total of 50 adults with sickle cell were screened as potential candidates for a half-matched stem cell transplant. After two unsuccessful attempts, scientists adopted the new protocol, which modifies one originally developed at Johns Hopkins University.
“We modified the transplant protocol by increasing the dose of radiation used before the transplant, and by infusing growth factor-mobilized peripheral blood stem cells instead of bone marrow cells,” Rondelli said. “These two modifications helped ensure the patient’s body could accept the healthy donor cells.”
Eight patients underwent the revised transplant. One developed chronic graft-versus-host disease, in which donor cells view the recipient’s cells as foreign and attack them, and died of what the researchers called “unknown causes” about one year post-transplant. The seven others were alive at a median follow-up of 16 months, and showed a stable 95% or greater acceptance (engraftment) of donor cells. These patients also show improved blood work at least one year following the transplant.
“These patients are cured of sickle cell disease,” Rondelli said. “This transplant protocol may cure many more adults patients with advanced sickle cell disease.”
But, they also warned, “Despite the increasing safety of the transplant protocols and new compatibility of HLA half-matched donors, many sickle cell patients still face barriers to care — of the patients we screened, only 20 percent underwent a transplant.”
Major factors limiting this transplant ranged from medical insurance denial, to personal decisions and high levels of donor antigens in patients who had received frequent blood transfusions, the study reported.
“The modified Hopkins regimen used here demonstrates high engraftment and low morbidity rates and should be tested in larger, multicenter, prospective clinical trials,” the researchers wrote.





