Sickle cell therapies, transplants need blood, platelet donations
American Red Cross to host more than 500 blood drives in September
Written by |
One sickle cell disease (SCD) patient may need as many as 50 units of blood and up to 25 units of platelets for the new cell-based gene therapies such as Casgevy and Lyfgenia to be successfully administered, according to the American Red Cross.
As a part of Sickle Cell Awareness Month, the Red Cross will host more than 500 blood drives nationwide to encourage blood and platelet donations to support those with sickle cell disease who are undergoing gene therapies and stem cell transplants, along with those who need regular blood transfusions to manage their disease and SCD-associated pain.
“Since the FDA approved these new cell-based gene therapies in December 2023, there has been a lot of excitement in both the sickle cell and medical community about the potential impact on the future health of patients,” Yvette Miller, MD, executive medical director of the American Red Cross, said in a press release. “However, what’s not being discussed is the crucial role blood donors will continue to play. Without their generosity, these treatments simply won’t be possible.”
SCD is an inherited disease caused by mutations in the HBB gene that cause an abnormal version of the protein hemoglobin that carries oxygen throughout the body to be produced. Blood cells with abnormal hemoglobin, known as hemoglobin S, become sticky, rigid and misshapen, taking on a distinctive sickle-shape. These sickled red blood cells cannot pass easily through small blood vessels, leading to blocked blood flow and other disease-related symptoms.
The U.S. Food and Drug Administration approved two new gene therapies, Casgevy and Lyfgenia for treating SCD late last year. Casgevy is intended to reduce the frequency and severity of vaso-occlusive crises, episodes of sudden, intense pain caused by the blockage of small blood vessels by sickle-shaped red blood cells. Lyfgenia both lessens the severity and frequency of vaso-occlusive crises and decreases acute chest syndrome and other sickle cell-related complications.
Increased need for blood, platelets
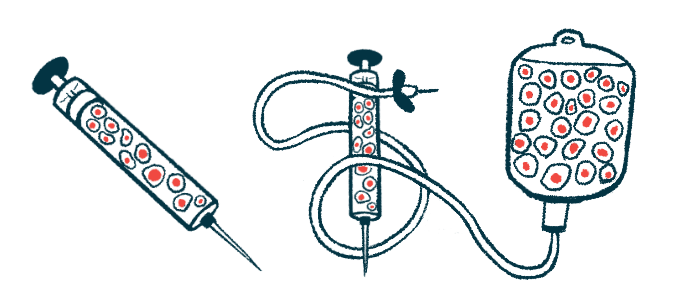
SCD patients who have gene therapy need blood and platelet transfusions before, during, and after treatment to ensure the best outcome. Blood transfusions are needed several months before gene therapy to maintain stable hemoglobin levels and ensure bone marrow health.
Both therapies require collecting a patient’s hematopoietic stem cells, that is, stem cell precursors that give rise to all mature blood cell types, and modifying them in a lab. Patients will also need blood cell exchanges, a nonsurgical therapy that removes unhealthy red blood cells and replaces them with healthy cells from donors. The modified cells are then returned to the patient via a stem cell transplant in a single intravenous infusion.
Patients are treated with a round of chemotherapy before a transplant to eliminate unhealthy blood cells with abnormal hemoglobin and make room for cells that have been modified by either gene therapy. During chemotherapy, red blood cells and platelet transfusions are needed to help carry oxygen and prevent complications, such as stroke.
Other available cures for SCD such as bone marrow and stem cell transplants also depend on blood and platelet donations. These cures rely on the availability of closely matched blood and platelet donations to reduce the risk of transfusion-related complications.
The likelihood of finding compatible blood donors for SCD patients is higher among people of Black or African American ethnicity, according to the Red Cross. In fact, these donors are nearly three times more likely to be a match for the specific blood type that’s frequently required, compared with donors from other ethnic backgrounds.
As sickle cell gene therapies and bone marrow and stem cell transplants evolve, the Red Cross views the efforts to maintain a robust supply of blood and platelet donations to be vital toward supporting treatment and ongoing care for patients who rely on regular blood transfusions to manage their disease.