Opioids for sickle cell disease
Last updated Aug. 14, 2024, by Lindsey Shapiro, PhD

What are opioids?
Opioids are a class of compounds with pain-relieving properties (analgesics) that are used for managing moderate to severe pain, including pain associated with sickle cell disease (SCD).
Several types of naturally occurring and lab-made (synthetic) opioids can be used for pain relief, and can be given in different strengths and through distinct routes of administration based on medical need.
But these compounds, including those used in medical settings, are highly addictive and come with some serious risks. Thus, they are generally reserved for treating pain that can’t be addressed by other means and should always be used exactly as prescribed by a medical professional. While most opioids have at least some medical uses, heroin is an illegal opioid that is not considered safe for any medical purpose and should never be used for pain relief.
When are opioids used in SCD?
Many SCD patients experience pain in some form, and opioids, given alongside other medications and interventions, are often central to its management. How opioids are used in SCD will depend on the type and severity of pain a patient is experiencing.
Acute pain
Acute bouts of severe pain are common in sickle cell disease, arising as a consequence of vaso-occlusive crises (VOCs). These episodes, often sudden and severe, occur when the abnormally shaped red blood cells that characterize SCD block blood vessels and compromise oxygen delivery to body tissues.
Opioids are often used in SCD for managing pain when it is moderate or severe. When patients arrive at a hospital or emergency department with a pain crisis, they’ll quickly be administered pain-relieving medications. The choice of whether to use opioids, and if so, the specific medication, dose, and route of administration, will be determined by a doctor based on the patient’s prior history and current pain severity.
In these instances, opioids are also commonly combined with other types of painkillers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), which typically are not addictive. This helps maximize pain relief with lower opioid doses.
Chronic pain
In addition to acute pain, SCD patients can experience chronic pain, which can be continuous or come and go, but is persistent over longer periods. The exact mechanisms underlying chronic pain in SCD are not completely understood. However, chronic pain can arise from secondary disease complications, such as bone degeneration or leg ulcers, or can be due to increased pain sensitivity without an identified cause.
While opioids may also be used to treat chronic pain, the benefits of their use for this purpose are not entirely clear. In fact, there is some evidence to suggest that long-term, high-dose usage of these medications could actually increase pain sensitivity. Moreover, because these therapies are highly addictive, there is greater abuse potential and risk of overdose when they are used over the long term.
Current guidelines suggest against chronic opioid therapy, unless the pain is not responsive to other treatment modalities. When long-term opioids are deemed necessary, they typically are prescribed at the lowest effective dose. If a person is exhibiting signs of opioid misuse or is responding poorly, the patient’s doctor may wean the individual off these medications in favor of nonopioid interventions.
How do opioids work?
Naturally-occurring opioids, also sometimes called opiates, come from the opium poppy plant and exert their effects on the body by binding to and activating opioid receptors. Synthetic opioids are lab-made versions designed to mimic the effects of the naturally-occurring substances.
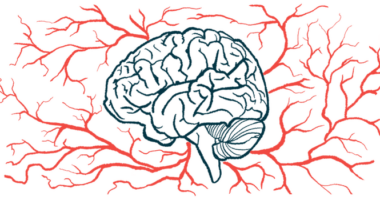
Pain is felt when certain nerve cells, including those in the spinal cord, send signals over to the brain. When opioids bind to opioid receptors on these nerve cells, they prevent them from sending such signals, thereby easing or eliminating perceptions of pain.
Dopamine, a brain chemical involved in feelings of pleasure and reinforcement, also is released when these receptors are activated. That release is what creates the euphoric sensation, or so-called high, that makes people enjoy the feeling of opioids, making them highly addictive.
There are three main types of opioid receptors — mu, kappa, and delta — each with slightly different biological effects. The most commonly prescribed opioids act on mu receptors, which have strong analgesic effects, but also mediate opioids’ addictive properties. Some medications will act, to varying degrees, on other opioid receptor types.
Opioid receptors in other areas of the body mediate other therapeutic effects of opioids, including diarrhea control.
Benefits of opioids
As strong pain relievers, opioids can help to significantly ease moderate or severe pain in SCD patients, especially when pain cannot be controlled by other types of medications or interventions. Opioids also come in formulations that allow for rapid pain relief, such as injections, which may be used when a person seeks treatment at a hospital for an acute and severe pain crisis.
The benefits of opioids for sickle cell disease have been demonstrated across various clinical trials involving adults and children with SCD.
Risks and side effects
Opioid side effects are very common, although the specific ones a patient experiences can depend on the potency of the product being used, its mode of administration, and the individual’s own tolerance to the medication. There also are certain serious risks associated with using opioids, especially if they are not used exactly as prescribed.
Variations in the genes encoding enzymes responsible for breaking down opioids can affect how sensitive a person is to the effects of these medications. Certain variations also can raise the risk that a person will experience severe or life-threatening events in response to opioids.
Side effects commonly observed with opioids when used as prescribed may include:
- drowsiness or sedation
- dizziness
- nausea and vomiting
- constipation
- respiratory depression (slow, shallow breathing).
Tolerance, dependence, addiction, and withdrawal
Over time, a person can build up a tolerance to opioids, whereby increasingly higher doses are required to achieve the same effects. This can ultimately give way to physical dependence, where the body is so used to the presence of the medications that it goes into withdrawal without them. This may lead individuals to continue using the medications to avoid those unwanted effects, driving opioid addiction.
Opioids are very addictive and are commonly misused or overused, even among people who were given a prescription for a legitimate medical purpose.
As such, opioids are highly regulated medications and a person’s need for them will be carefully considered by the individual’s doctors and broader healthcare team. Even when they’re deemed necessary, the goal is for patients to use the lowest possible dose over the shortest period of time. Patients should always use opioids exactly as they were prescribed.
If a person has been taking opioids for a length of time, the individual’s body might go into withdrawal when stopping treatment. This can come with symptoms including agitation, anxiety, insomnia, and gastrointestinal distress. For those reasons, opioids generally should not be stopped suddenly and should be tapered off under medical supervision.
Respiratory depression and overdose
Because opioids act on parts of the brain that control breathing, they can slow breathing down. It is possible that breathing may become so slow that a person experiences brain hypoxia, where too little oxygen reaches the brain, which is life-threatening. People with certain lung conditions may be at a higher risk for this complication.
This issue is also more likely to occur when opioids are used more often or at higher doses than they should be, and respiratory depression is generally the cause of death from an opioid overdose.
Opioids generally should not be combined with alcohol or other medications that also slow breathing rates, as this can lead to life-threatening interactions. Patients should discuss all substances they are using with their doctor.
Pregnancy and breastfeeding
Opioids are generally not recommended for women who are pregnant, as a developing fetus can become physically dependent on opioids while in the womb. Subsequent withdrawal symptoms in the baby after birth may include irritability, seizures, fever, or poor feeding. Other birth defects, stunted growth, and premature delivery are also risks of opioid use during pregnancy.
SCD patients using opioids for pain management should always talk to their doctor if they plan to become pregnant or are already pregnant. Suddenly stopping these medications can cause severe health problems, so patients and their doctors should come up with the safest possible plan for both the individual mother and child.
Opioids also can pass into breast milk, so nursing patients should talk with their doctors if they wish to breastfeed while using these medications.
Opioids used in SCD
While all opioids have a generally similar mechanism, some have stronger pain-relieving properties than others. Both weak and strong opioids are used in different scenarios to manage SCD-related pain.
Specific opioid side effects and risk profiles also may depend on the strength of the medication being used. A person’s doctor will determine which opioids are best based on the patient’s individual case.
Weak opioids
In general, weaker opioids have less potent analgesic properties, and thus are used to treat moderate pain in SCD patients.
Several opioids in this class may be used for managing SCD:
- Codeine (sold as Tuxarin ER) is a naturally occurring opioid that’s also a component of common cold and flu medicines. This medication is most commonly available in oral formulations (tablets, capsules, or solutions) alone or as a combination product containing other analgesics.
- Tramadol (sold as Conzip and others) is a synthetic opioid most commonly taken in oral formulations, including extended-release formulations. It’s also available in combination with nonopioid pain-relieving medications.
- Hydrocodone (sold as Hycodan and others) is a synthetic codeine derivative that’s commonly sold in combination with other analgesics. It is available in several oral formulations.
Strong opioids
Strong opioids have greater pain-relieving abilities, and as such, are used to treat more severe pain in SCD patients. Due to their stronger effects, these medications are also more likely to be abused and may come with a higher risk of overdose.
There are many types of strong opioids a doctor might prescribe for SCD pain management:
- Morphine (sold as Duramorph PF and others) is a widely known, naturally occurring opioid that’s commonly prescribed in SCD. It’s available in various formulations, including oral and injectable. A number of other opioid medications are derivatives of morphine.
- Fentanyl (sold as Actiq and others) is a very potent synthetic opioid — as much as 100 times more potent than morphine — used for severe pain. It comes in the form of oral tablets, injections, lozenges, oral films, and skin patches.
- Oxycodone (sold as Oxycontin and others) is another synthetic opioid, one available in both extended-release and immediate-release oral capsules or solutions. It sometimes also comes as a combined product with nonopioid painkillers.
- Levorphanol (available as generics) is a synthetic opioid initially developed as a more potent and longer-acting alternative to morphine. This medication is used orally in SCD to treat moderate to severe chronic pain, or in combination with short-acting opioids for acute pain relief.
- Methadone (sold as Methadose) is a long-lasting synthetic opioid used for severe pain. It’s available in oral or injectable formulations. Methadone also is used to help eliminate symptoms of withdrawal and craving when a person is trying to quit using heroin or other opiates.
- Hydromorphone (sold as Dilaudid) is a synthetic and more potent morphine derivative with quick-onset relief for severe pain. It is available in oral and injectable formulations.
- Meperidine (sold as Demerol) is another synthetic opioid, one that’s available in oral and injectable formulations.
Sickle Cell Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Gene-editing therapy may cut stroke risk in SCD, small study finds
- Dosing started in Phase 1 study of globin-switching therapy CLY-124
- What I’ve learned about life, love, and sacrifice due to caregiving
- ED pain scores may predict future hospitalization for SCD children
- What to consider before making a change to your treatment regimen
- Buprenorphine may reduce opioid use for sickle cell disease patients
- Reflecting on 4 years of sharing my experiences with sickle cell
- Level of physical activity tied to less pain, blood viscosity in SCD: Study
- Celebrating ourselves is a way to promote sickle cell awareness
- BEAM-101 shows sustained benefits as treatment for sickle cell
Related articles